Thank you for your request!
We appreciate your interest in Health Testing Solutions! We will get back to you as soon as possible.
In the meantime, our FAQs below may provide answers to some of your questions. We look forward to talking with you!
General FAQs
Yes. We offer nationwide services. We have mobile units strategically positioned throughout the country. In some markets, we utilize our network to help support remote areas or supplement our existing mobile units.
We continue to be an industry leader in on-site mobile hearing testing, audiometric data management, qualitative and quantitative respirator fit testing, and physical examinations designed for OSHA, MSHA, DOT, and governmental agency regulatory compliance and occupational health surveillance programs.
Our founder, Johnny L. Sanders, Audiologist, started his first occupational medical company in 1979. From there, Johnny pioneered the deployment of on-site mobile medical surveillance services nationwide. He remains active with business development projects and continues to support customers with Professional Supervisor Services.
Yes. We are aware that our customers have unique needs. Our field operations staff accommodate requests to cover multiple shifts, holidays, and weekends.
No, not currently. We only offer on-site mobile testing services.
No. We bill employers directly for our services.
Pricing is generally based on a combination of several factors, such as: (i) the anticipated number of people to receive each service, (ii) the expected number of hours or days we are requested to be on-site, (iii) the customer location, (iv) travel time or mobilization considerations, and (v) urgency to schedule. The best approach is to connect with our Sales Team and discuss your unique scheduling needs.
Our goal is to meet the time constraints of our customers every time. Depending on the service requested, we may have immediate availability on short notice. The best approach is to connect with our Sales Team and discuss your unique scheduling needs.
Yes. We have multiple Board-Certified Occupational Medicine Physicians available to conduct on-site physical examinations and to support customer inquiries during normal business hours.
Yes. We have multiple experienced Industrial Audiologists on staff. Our Audiologists are available to support your hearing conservation program questions, evaluate standard threshold shifts, and make professional recommendations regarding work-related hearing loss cases.
Mobile Hearing FAQ
Our 8-booth audio-only mobile units can test up to 8 workers every 20 minutes or up to 24 workers per hour. Our 6-booth audio-only mobile units can test up to 6 workers every 20 minutes or up to 18 workers per hour.
Yes. Hearing History Questionnaires are made available to workers prior to testing.
Yes. Otoscopic exam results are documented on the Hearing History Questionnaire upon entering the mobile testing unit.
We utilize instantaneous sound level meter devices in our mobile units. If at any time noise inside of the testing booth exceeds OSHA permissible ambient limits, our audiometers do not record a test value. Our sound level meters meet the ANSI requirements for both a Type 2 Octave Band Filter and a Type 2 Sound Level Meter and therefore help testing always remain compliant.
Yes. Our microprocessor audiometers can give instructions in over 50 languages including Spanish, Vietnamese, Chinese, French, Arabic, Korean and German.
According to OSHA, “…audiometric tests shall be performed by a licensed or certified audiologist, otolaryngologist, or other physician, or by a technician who is certified by the Council of Accreditation in Occupational Hearing Conservation, or who has satisfactorily demonstrated competence in administering audiometric examinations, obtaining valid audiograms, and properly using, maintaining and checking calibration and proper functioning of the audiometers being used. A technician who operates microprocessor audiometers does not need to be certified. A technician who performs audiometric tests must be responsible to an audiologist, otolaryngologist or physician…”
Yes, we comply 100% with this requirement. In fact, while we do exclusively utilize microprocessor audiometers, we still require our technicians to be CAOHC certified. Furthermore, all technicians are responsible to our Professional Team which includes both Audiologists and Physicians.
Our audio-only mobile units require single-phase, 50AMP, 120V/240V, 4-wire power.
Yes. Our audiometric testing mobile units are pulled by trucks with on-board generators.
We prefer to use power supplied by our customers when it is available. If the appropriate outlet is installed prior to testing or already exists, then everything should be plug-and-play. Before energizing the trailer, however, we ask that an electrician onsite verifies outlet polarity, voltage, and amperage. Our mobile units require single-phase, 50AMP, 120V/240V, 4-wire power.

The preferred outlet is a NEMA 14-50R.
Yes. All mobile units have pigtails available for an onsite electrician to wire into a breaker box with single-phase, 50AMP, 120V/240V, 4-wire power.
Typically, there is no pain, no visible trauma, no scarring, may take years to diagnose, and is GRADUAL, PERMANENT, and 100% PREVENTABLE.
People with hearing loss experience various levels of disruption in relationships, may have a loss of self-confidence, are sometimes confused or impatient, have an increased stress level or sense of fatigue, may find others talking down to them, or may find group activities less enjoyable.
Respirator Fit Testing FAQs
29 CFR 1910.134
A fit test is conducted to verify that a respirator is both comfortable and correctly fits the user. Fit test methods are classified as either qualitative or quantitative. A qualitative fit test is a pass/fail test that relies on the individual’s sensory detection of a test agent, such as taste, smell, or involuntary cough. A quantitative fit test uses an instrument to numerically measure the effectiveness of the respirator.
The employer shall ensure that an employee using a tight-fitting facepiece respirator is fit tested prior to initial use of the respirator, whenever a different respirator facepiece (size, style, model or make) is used, and at least annually thereafter.
The employer shall conduct an additional fit test whenever the employee reports, or the employer, PLHCP, supervisor, or program administrator makes visual observations of, changes in the employee's physical condition that could affect respirator fit. Such conditions include, but are not limited to, facial scarring, dental changes, cosmetic surgery, or an obvious change in body weight.
If after passing a QLFT or QNFT, the employee subsequently notifies the employer, program administrator, supervisor, or PLHCP that the fit of the respirator is unacceptable, the employee shall be given a reasonable opportunity to select a different respirator facepiece and to be retested.
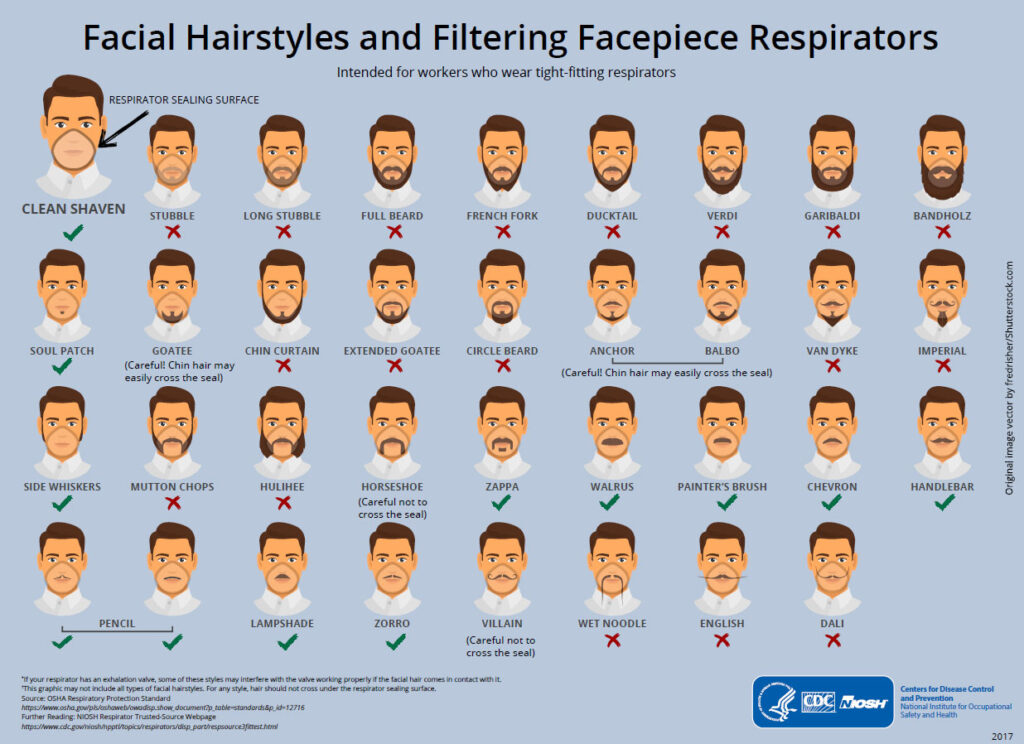
The employer shall not permit respirators with tight-fitting facepieces to be worn by employees who have:
- Facial hair that comes between the sealing surface of the facepiece and the face or that interferes with valve function; or
- Any condition that interferes with the face-to-facepiece seal or valve function.
NIOSH has published the following infographic to help employers educate employees about acceptable facial hair while using tight-fitting respirators:
Yes. If we have the masks requested in inventory, we will supply them for fit testing. Otherwise, we can source masks upon customer request.
We recommend, especially since the COVID-19 Pandemic, that employees fit test on their own dedicated respirators. However, this is not always feasible for employers. For non-filtering facepiece respirators such as elastomeric half and full facepieces that may be shared during fit testing, we recommend that employees follow the appropriate cleaning procedures as outlined by their employers’ workplace respiratory protection program and follow guidance from OSHA, EPA, CDC, NIOSH and respirator manufacturers. Specifically, at the end of each day, employers should follow Appendix B-2 of 1910.134: Respirator Cleaning Procedures (Mandatory). While OSHA allows employers to use towelettes between employees during fit testing, we urge extra caution with this approach due to the infectious nature of respiratory diseases such as COVID-19. Our technicians are not responsible for cleaning respirators between each use, even if we supply respirators for fit testing purposes.
Yes. However, this interpretation has not been updated since 1999. Click here to read the interpretation published on OSHA’s website regarding towelettes.
Yes. We can fit test using the employees’ own respirator.
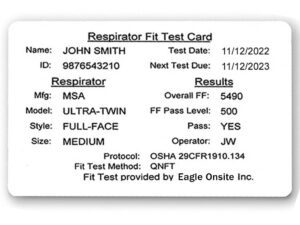
Yes. A card is printed immediately upon successful completion of the respirator fit test and given to the employee. The card provides documentation of the completed fit test and easy field verification of proper respirator size and model for the authorized respirator user.
We can scale appropriately to meet your needs. If time is tight, we will staff more equipment and more personnel to help reduce employee time away from work. Speak with our Sales Team to discuss the optimal balance of fit testing resources to meet any scheduling constraints.
This topic is rather extensive. Review the interpretation letter to the standard found here for more information on this topic.
A user seal check is mandatory for individuals using a tight-fitting respirator. Review Appendix B-1 to section 1910.134 here for further information regarding User Seal Check Procedures(Mandatory).
Yes. To review Appendix A to section 1910.134 – Fit Testing Procedures (Mandatory), click here.
Respirator Medical Evaluation FAQ
Yes. We offer several methods for employees to obtain respirator medical clearance, including an Online Option and Paper Option.
Yes. A link is always available at the upper right-hand corner of our website.
Pricing varies based on volume. Contact our Sales Team today for pricing.
Respiratory Program Administrators are provided unique admin user instructions and unique employee user instructions. Employees can log in during their normal working hours or at a time and place convenient to them to complete the questionnaire online. Questions are presented one-at-a-time as not to overwhelm employees. Upon completion of the questionnaire, employees are immediately presented with a status of either clear, pending review, or not qualified. Contact our Sales Team to establish a new company account or demo our online application.
Using a respirator may place a physiological burden on employees that varies with the type of respirator worn, the job and workplace conditions in which the respirator is used, and the medical status of the employee.
The employer shall identify a physician or other licensed health care professional (PLHCP) to perform medical evaluations using a medical questionnaire or an initial medical examination that obtains the same information as the medical questionnaire. The employer shall ensure that a follow-up medical examination is provided for an employee who gives a positive response to any question among questions 1 through 8 of the respirator medical evaluation questionnaire. The follow-up medical examination shall include any medical tests, consultations, or diagnostic procedures that the PLHCP deems necessary to make a final determination. This may be a simple phone call to verify a response.
The medical questionnaire and examinations shall be administered confidentially during the employee's normal working hours or at a time and place convenient to the employee. The medical questionnaire shall be administered in a manner that ensures that the employee understands its content.
Employees may contact our medical department during normal business hours for support. A medical team representative will help facilitate the discussion.
No. Forms which are intended to gather an employee's medical history prior to receiving a physical examination by a PLCHP may be designed to suit the PLCHP and do not have to follow the respirator questionnaire presented in Appendix C of the 1910.135 standard. Any information not included in the form can be gathered by the PLCHP during the physical examination.
The written recommendation from the Eagle Onsite PLHCP includes any limitations on respirator use related to the medical condition of the employee or relating to the workplace conditions in which the respirator will be used, including whether or not the employee is medically able to use the respirator; the need, if any, for follow-up medical evaluations; and a statement that the PLHCP has provided the employee with a copy of the PLHCP's written recommendation.
If an employee reports medical signs or symptoms that are related to ability to use a respirator; a PLHCP, supervisor, or the respirator program administrator informs the employer that an employee needs to be reevaluated; information from the respiratory protection program, including observations made during fit testing and program evaluation, indicates a need for employee reevaluation; or a change occurs in workplace conditions (e.g., physical work effort, protective clothing, temperature) that may result in a substantial increase in the physiological burden placed on an employee, then additional medical evaluation is appropriate.
No. However, when additional follow-up is appropriate, the follow-up medical examination may include any medical tests, consultations, or diagnostic procedures that the PLHCP deems necessary to make a final determination. This may or may not include a pulmonary function test. Review the interpretation letter to the standard found here for more information on this topic.
Physical Examination FAQ
Yes. We bring all necessary equipment and personnel directly to your worksite.
While we can scale up or down to meet demand, we base the number of employees to be seen per hour on how many practitioners we provide onsite and the type of physical exam we are asked to provide. One practitioner can easily examine one worker every 10-15 minutes. Our practitioners understand the value of employee time away from work. Each employee exam will be thorough and will include time to discuss exam results confidentially with our practitioner.
No. However, some exams do require fasting. When fasting is necessary, our team will provide appropriate instructions in advance.
Yes. We have DR X-Ray systems on all physical exam mobile units.
Yes. We have several NIOSH Certified B-Readers available to interpret X-Rays and report appropriately.
Our physical exam mobile units are powered with bumper-pull diesel generators. In some cases, we supply power. In other cases, our customers provide power. During the quotation process, this component is addressed.
Pulmonary Function Testing FAQs
On average, a PFT requires about 10 minutes to complete. Some exam sessions take less time, while others require more time. The duration of each exam session is mainly dependent on successful coaching by our NIOSH Certified technicians and the acceptable, repeatable efforts by the employee. Appropriate rest is provided between maneuvers so that employees may recover and repeat test efforts to the best of their ability.
Yes. In fact, we are unable to begin testing without a passing daily calibration check.
A pulmonary function test is often utilized for industrial screening and surveillance purposes. Many OSHA medical surveillance provisions require a pulmonary function test such as Respirable Crystalline Silica, Asbestos, Benzene and Formaldehyde.
No. A PFT is not a requirement for determining respirator clearance. Review the interpretation letter to the 1910.134 respiratory protection standard found here for more information on this topic.
Yes. In fact, we are also a NIOSH Certified Spirometry Facility.
Yes. Click here to review the document published in 2011.
Yes. Click here to review the document published in 2011.
Professional Supervisor Services FAQs
OSHA’s Hearing Conservation Amendment 29 CFR 1910.95 states that a technician who performs audiometric tests must be responsible to an audiologist, otolaryngologist, or physician. Furthermore, the audiologist, otolaryngologist or physician shall review problem audiograms and shall determine whether there is a need for further evaluation.
We have experienced Audiologists and Physicians capable of making determinations of work-relatedness for noise induced hearing loss who are also responsible for overseeing our mobile technicians.
Yes. We always maintain at least one Audiologist or Physician who has completed the one-day training program to become a CAOHC Certified Professional Supervisor of the Audiometric Monitoring Program©.
Our STS Tracking System™ is a comprehensive reporting system designed to streamline management of problem audiograms and guide employers through the work-related determination process when necessary. We understand that following up with problem audiograms can be frustrating for employers, especially in a dispersed workforce. Our proprietary STS Tracking System™ helps employers remain in compliance while focusing attention on exactly what is needed in a step-by-step guide from start to finish.
STS is short for Standard Threshold Shift. A Standard Threshold Shift, or STS, is defined in the occupational noise exposure standard at 29 CFR 1910.95(g)(10)(i) as a change in hearing threshold, relative to the baseline audiogram for that employee, of an average of 10 decibels (dB) or more at 2000, 3000, and 4000 hertz (Hz) in one or both ears.
Click here for the recording criteria as outlined in OSHA 29 CFR 1904.10.
If an employee's hearing test (audiogram) reveals that the employee has experienced a work-related Standard Threshold Shift (STS) in hearing in one or both ears, and the employee's total hearing level is 25 decibels (dB) or more above audiometric zero (averaged at 2000, 3000, and 4000 Hz) in the same ear(s) as the STS, you must record the case on the OSHA 300 Log.
Furthermore, a physician or other licensed health care professional must determine if the hearing loss is in fact work-related using rules set forth in section 1904.5. If an event or exposure in the work environment either caused or contributed to the hearing loss, or significantly aggravated a pre-existing hearing loss, you must consider the case to be work related.
According to OSHA, if a physician or other licensed health care professional determines, following the rules set out in section 1904.5, that the hearing loss is not work-related or that occupational noise exposure did not significantly aggravate the hearing loss, you do not have to consider the case work-related or record the case on the OSHA 300 Log.
Click here to review the National Hearing Conservation Association (NHCA) guidance on determining work-relatedness and wording determinations for reports, published in 2011.
We practice ethical, professional objectivity when presenting medical-legal reports. Our Professional Supervisor Services Team understands the “more probable than not” requirement and is experienced in applying informed professional judgment with work-relatedness determinations. Our professionals do not represent the employee, employers, or OSHA.
We are your partner during OSHA audits. One role of our Audiologists and Physicians is to support all parties with explaining outcomes addressing whether a work exposure either caused or contributed to the hearing loss or significantly aggravated a pre-existing hearing loss, or if an exception specifically applies. When we are in the role of Professional Supervisor for a Hearing Conservation Program, our professional consulting services are available throughout the year, on-demand.
According to MSHA, a change in hearing sensitivity for the worse, relative to the miner's baseline audiogram, or the miner's revised baseline audiogram where one has been established in accordance with section 62.170(c)(2), of an average of 25 dB or more at 2000, 3000, and 4000 Hz in either ear.
Click here for the recording criteria as outlined in MSHA 30 CFR Part 62.
CWHS FAQs
Yes. The National Institute for Occupational Safety and Health (NIOSH) in Morgantown, West Virginia, administers the CWHSP which is a congressionally-mandated medical examination surveillance program for monitoring the health of coal miners. The CWHSP was originally authorized under the 1969 Federal Coal Mine Health and Safety Act and is currently authorized under the 1977 Federal Mine Safety and Health Act and its subsequent amendments.
No. Miner participation is voluntary. However, NIOSH recommends both a chest radiograph and a spirometry examination every 4 to 5 years for the first 15 years of coal mining and every 3 years after that if the miner remains engaged in coal mining.
No. Miners may request medical examinations at the expense of their employer.
Only one (1) PA Chest X-Ray is acquired during the medical examination.
Yes. Each participating miner must complete the Miner Identification Document. For spirometry tests, the Spirometry Results Notification Form and the Respiratory Assessment Form must be completed.
No. Per the guidelines in the CWHSP, we are NOT PERMITTED to retain any records of the miner medical examination. All data is forwarded within two (2) weeks to NIOSH.
No.
It is helpful for the mine operator or contractor to provide the names and addresses of miners who may come in to be examined.
No.
An Eagle Onsite designated Physician performs a “facility” reading of the Chest X-Ray and Spirogram obtained from the miner. Physician comments are reported to NIOSH. If the Eagle Onsite designated Physician documents any abnormalities from the Chest X-Ray that require the miner follow up with their Physician (specifically, this is noted in section 4E of the Chest Radiograph Classification Form CDC/NIOSH 2.8), then the Eagle Onsite medical department will notify the miner of the findings by either USPS mail or secure email and reports the notice of communication to NIOSH.
